What is the Measurable Activities & Participation System (MAPS)?

A Smarter Starting Point Before the Metrics Begin
Medicare Advantage plans are under increasing pressure to improve CMS Star Ratings while delivering stronger member engagement—and that’s where MAPS begins.
Measurable Activities & Participation System (MAPS) is Patient Better’s proprietary quality and engagement suite designed to activate member behavior before it affects CAHPS or HEDIS performance.
MAPS helps Medicare Advantage plans improve Star Ratings by preparing members to engage early—before performance is measured.
We provide a structured, measurable system that:
- Activates member behavior from day one
- Supports follow-through on care plans, screenings, and instructions
- Documents engagement—whether a member participates, declines, or doesn’t respond
- Aligns with CMS priorities for quality, equity, and audit-readiness
- Integrates without adding staff, tech, or clinical burden
In short, we help you influence what happens before CAHPS and HEDIS scores are locked in—when it still counts.
MAPS Starts on Day One—So Your Quality Strategy Doesn’t Fall Behind
🔠 Official Definition for MAPS
MAPS: Measurable Activities & Participation System
A proprietary pre-measurement solution that empowers Medicare Advantage plans to engage beneficiaries in their care before measurement interventions begin.
Traditional engagement tools focus on tracking member behavior after the fact. MAPS is different. It activates and prepares members before performance is measured—at enrollment, re-enrollment, or any strategic touchpoint.
By offering a structured, reportable path from the first point of contact, MAPS helps plans shape behavior early, close compliance gaps, and produce documentation that stands up to CMS expectations.
With MAPS, your plan can:
- Strengthen Star Ratings by influencing behavior before CAHPS and HEDIS are measured
- Track and document member engagement from day one
- Cut through noise with a structured system—not just fragmented outreach
- Equip members with guided tools that build trust and follow-through
- Generate audit-ready documentation—whether members engage, decline, or don’t respond
Why Choose MAPS
✅ Drives Higher Star Ratings Improves CMS performance by preparing members in advance—boosting preventive care, adherence, and CAHPS scores while reducing complaints.
✅ Self-Guided, Zero-Lift Implementation
Empowers members to manage their care independently, while your team benefits from a plug-and-play system with no added staffing or training.
✅ Built-In Documentation for Compliance
Generates measurable engagement data to support audits, risk adjustment, and CMS reporting—fully aligned with quality initiatives.
✅ Closes Gaps Before They Cost You
Helps members follow through on screenings, medications, and care plans—preventing missed measures and downstream penalties.
✅ Increases Member Satisfaction & Loyalty
Strengthens retention by turning passive beneficiaries into proactive participants, making your plan the obvious top-tier choice.
Why MAPS Works: The Science Behind It
MAPS (Measurable Activities & Participation System) is a proprietary, pre-measurement solution that helps Medicare Advantage plans improve Star Ratings by addressing a core system gap: unprepared members.
While CAHPS and HEDIS measure what members think and how providers perform, MAPS works upstream—training and activating members before those metrics are triggered. This proactive engagement reduces risk, improves outcomes, and ensures your plan is positioned for long-term quality success.
🔍 Key Features:
- Improves CMS performance by preparing members to follow through with care before they’re scored
- Generates measurable behavioral data to support audits, risk adjustment, and quality reporting
- Strengthens CAHPS, HEDIS, and health equity efforts through targeted engagement
- Deploys without burdening staff or systems, making it easy to implement and scale
What Medicare Advantage Plans Need to Know About MAPS
MAPS improves Star Ratings by addressing a gap neither HEDIS nor CAHPS fully solve—member preparedness.
Most Star Ratings issues stem not from poor care delivery, but from members who are confused, disengaged, or unready to follow through. MAPS changes that by activating members before they interact with the system. It teaches them how to communicate with providers, follow instructions, and manage their care—resulting in:
- Higher CAHPS scores through better experiences and reduced complaints
- Cleaner HEDIS outcomes through fewer missed appointments, screenings, or refills
- Improved adherence and satisfaction that boosts both quality and retention
Because MAPS includes tools to measure behavior change and readiness, it also gives your plan documentable proof that member engagement is happening—supporting your CMS quality strategy.
In short: MAPS turns hard-to-reach members into better healthcare participants, which leads directly to better performance scores.
MAPS fills the upstream gap in your quality strategy—before CAHPS and HEDIS are triggered.
While your current tools measure provider performance (HEDIS) and member perception (CAHPS), MAPS focuses on preparing the member before either of those metrics apply. It supports the front end of your care model by teaching members how to participate effectively—so by the time they’re measured, they’re already engaged, informed, and more likely to follow through.
MAPS doesn’t replace your existing systems—it strengthens them. It integrates alongside your current engagement, care coordination, and quality improvement efforts without requiring additional technology, workflow changes, or staff training.
Think of it as the first step in your performance pipeline—a lightweight, scalable layer that improves everything that follows.
Yes. MAPS directly supports multiple CMS requirements tied to Star Ratings, member engagement, and health equity.
By activating members before they’re measured, MAPS helps your plan:
- Improve CAHPS scores through better communication, care coordination, and patient understanding
- Support HEDIS goals by helping members follow through on screenings, medications, and preventive services
- Meet CMS health equity expectations by delivering accessible, self-guided education that closes literacy and access gaps
- Demonstrate proactive engagement using built-in tools like the Readiness Assessment and Completion Survey
MAPS is designed to be low-lift and fully independent of your internal systems, teams, and workflows.
There is no integration required, and it doesn’t involve your EHR, IT, or clinical staff. The program is self-guided for members and fully managed by Patient Better.
Here’s what that means for your organization:
- No provider training or clinical workflow disruption
- No new technology platforms to adopt or configure
- No additional staff or FTEs needed to launch or maintain it
- No data sharing obligations—we handle all participation, assessments, and engagement tracking on our side
You simply license the program, offer it to your members, and receive measurable, documented results. We designed MAPS to be plug-and-play so your plan can improve Star Ratings without adding complexity.
MAPS tracks member participation and documents change through a structured system anchored by a formal intervention, supported by built-in evaluation tools.
When a Medicare Advantage plan deploys MAPS, each member receives an invitation to participate. From there, they have three options:
- No Response: The member ignores the invitation. No action is taken, and the plan is not charged.
- Signs Non-Compliance Waiver: The member begins the process but chooses not to continue. Their opt-out is formally documented, giving your plan audit-ready evidence that support was offered.
- Full Participation: The member completes the MAPS system, including the intervention, and their behavior change is documented for reporting and performance purposes.
Why It Matters for CMS Reporting:
Regardless of which path the member chooses, MAPS provides reportable documentation that can support your CMS-facing quality strategy. If a member later receives a poor HEDIS or CAHPS score, your plan can show that:
- An engagement program was offered
- Support was made available
- The member’s decision and level of participation were documented
This creates a protective compliance layer and strengthens your ability to report on quality improvement, health equity efforts, and member outreach—all tied to Star Ratings performance.
In all cases, MAPS ensures your plan is never charged for what members don’t do—while still protecting you with compliance-ready documentation.

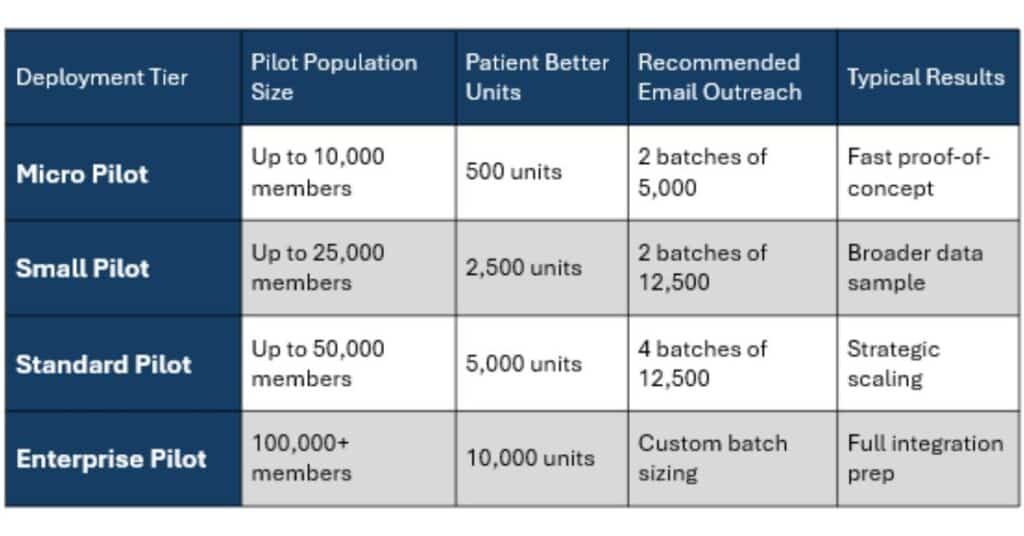
📈 Plan Calculator
Choose your pilot size. Deploy Patient Better. Get measurable results.
Patient Better is a ready-to-deploy intervention that teaches beneficiaries how to navigate their healthcare. Your plan only pays for units shipped. However, you receive an outcome for every member contacted—giving you full visibility into engagement and activation.
What Happens Next?
Once email invitations are sent, members fall into one of four documented categories:
- No Response: Email was unopened or ignored. No charge.
- Challenge Only: Member took the Healthcare Proficiency Challenge but did not proceed. No charge.
- Waiver Submitted: Member acknowledged the offer and declined to move forward by submitting a Non-Compliance Waiver.
- Program Enrolled: Member requested and received a Patient Better unit. This is a billable engagement and is counted toward your total unit allocation.
What You Get
- You only pay for shipped units (actual program participants).
- You receive data on all outreach outcomes, even for non-participants.
- You gain real behavioral insights—including activation rates, opt-out documentation, and completion metrics.
- You control scale—start with a micro pilot, expand only if desired.
Why It Works
- Zero-risk entry point
- Immediate CMS-aligned data on engagement
- Budget-predictable: You’re not charged until a member engages
- Built for fast deployment—no workflow disruption
Ready to See MAPS in Action?
If your Medicare Advantage plan is looking for a measurable, low-lift way to support member engagement, improve Star Ratings, and meet CMS goals—MAPS is ready when you are.
Book a brief demo to see how the system works and whether it’s the right fit for your quality strategy.
No obligation—just clarity.
Disclaimer: This education was brought to you today by The Patient Better Project Inc., a 501(c)(3) organization dedicated to reshaping the way patients and caregivers navigate care. We are committed to empowering individuals with the knowledge and tools necessary to take control of their health journeys, ensuring that everyone can access the care they need with confidence and clarity.
The information provided here is for educational and entertainment purposes only. It is not intended as, nor should it be considered a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call 911 or your local emergency number.