Incredible Healthcare Challenges: How "Difficult Patients" Navigate Tough Situations to Improve Their Care Experience

Patients and caregivers also ask
Understanding and addressing difficult patient behaviors in healthcare is crucial for several reasons:
Improved Patient Outcomes: By recognizing and addressing the root causes of difficult behaviors, healthcare providers can tailor their approach to meet the specific needs of these patients, leading to better health outcomes.
Enhanced Communication: Addressing difficult behaviors fosters open and effective communication, which is essential for accurate diagnoses, treatment adherence, and overall patient satisfaction.
Increased Efficiency: Understanding and managing difficult patient behaviors can reduce the time and resources spent on misunderstandings and non-compliance, allowing for more efficient and productive medical appointments.
Stronger Patient-Provider Relationships: Proactively addressing difficult behaviors helps build trust and collaboration between patients and healthcare providers, leading to a more positive and cooperative healthcare experience.
Reduced Stress for Healthcare Providers: When difficult patient behaviors are understood and managed effectively, it reduces stress and burnout among healthcare providers, enabling them to deliver higher quality care.
Overall, understanding and addressing difficult patient behaviors is essential for creating a more effective, efficient, and empathetic healthcare system that benefits both patients and providers.
Addressing the needs of difficult patients can significantly improve outcomes for both patients and caregivers in several ways:
Enhanced Patient Engagement: Educating and empowering difficult patients can transform them into proactive partners in their healthcare journey, leading to better adherence to treatment plans and improved health outcomes.
Better Communication: Addressing difficult behaviors fosters open and effective communication, ensuring that patients understand their conditions and treatment options, which is crucial for making informed healthcare decisions.
Reduced Stress for Caregivers: When difficult behaviors are managed, caregivers experience less stress and frustration, allowing them to provide more focused and effective care.
Increased Efficiency: Managing difficult patient behaviors reduces the administrative burden on healthcare providers, making appointments more productive and allowing for more personalized care.
Stronger Patient-Provider Relationships: Proactively addressing the needs of difficult patients builds trust and collaboration, leading to a more positive and cooperative healthcare experience for all parties involved.
By addressing the needs of difficult patients, healthcare systems can create a more supportive and efficient environment that benefits both patients and caregivers.
Understanding difficult patients offers several key benefits:
Improved Patient Outcomes: Recognizing and addressing the behaviors of difficult patients allows healthcare providers to tailor their care strategies, leading to better health outcomes and enhanced treatment adherence.
Enhanced Communication: Understanding the root causes of difficult behaviors promotes more effective communication, ensuring that patients receive clear, comprehensible information about their health and treatment options.
Increased Efficiency: By managing difficult behaviors effectively, healthcare providers can reduce time and resource wastage, making medical appointments more efficient and productive.
Reduced Caregiver Stress: Caregivers experience less stress and frustration when they understand and can manage difficult patient behaviors, enabling them to provide higher quality care.
Stronger Patient-Provider Relationships: A deeper understanding of difficult patient behaviors fosters trust and collaboration, leading to stronger and more cooperative relationships between patients and healthcare providers.
Enhanced Patient Satisfaction: Patients who feel understood and properly managed are more satisfied with their care, which can improve their overall healthcare experience and outcomes.
Overall, understanding difficult patients is essential for creating a more empathetic, effective, and efficient healthcare system that benefits both patients and caregivers.
Difficult patients can contribute to effective health management in several ways when their behaviors are understood and appropriately addressed:
Improved Tailoring of Care: Recognizing the specific needs and behaviors of difficult patients allows healthcare providers to tailor their care strategies, ensuring that each patient receives personalized and effective treatment.
Enhanced Patient Engagement: Addressing the root causes of difficult behaviors can transform these patients into more active and engaged participants in their healthcare, leading to better adherence to treatment plans and improved health outcomes.
Better Communication: Understanding difficult patient behaviors promotes open and honest communication. This ensures that patients fully understand their conditions and treatment options, leading to more informed decision-making and better management of their health.
Increased Efficiency: Effectively managing difficult patient behaviors reduces misunderstandings and non-compliance, making medical appointments more efficient and productive. This allows healthcare providers to focus on delivering high-quality care.
Stronger Relationships: Addressing the needs of difficult patients helps build trust and cooperation between patients and healthcare providers, fostering stronger and more collaborative relationships that are essential for effective health management.
Empowerment and Education: Programs like Patient Better’s Health Advocacy Program can educate and empower difficult patients, providing them with the knowledge and tools they need to manage their health more effectively and become proactive healthcare partners.
Overall, by understanding and managing difficult patient behaviors, healthcare providers can create a more supportive and efficient environment, leading to more effective health management and better outcomes for both patients and caregivers.
Patients and caregivers should learn about difficult patients for several important reasons. Understanding the behaviors and challenges of difficult patients can help improve communication, ensuring that important health information is accurately conveyed and understood. It leads to more personalized and effective care plans, improving overall health outcomes for patients. By recognizing the reasons behind difficult behaviors, whether they stem from fear, anxiety, lack of knowledge, or previous negative experiences, caregivers and healthcare providers can manage these situations more calmly and efficiently, reducing stress and frustration for everyone involved.
This knowledge fosters trust and cooperation, leading to stronger and more positive relationships. It also empowers patients and caregivers to become more proactive in managing healthcare interactions, advocating for better care and support. Addressing difficult behaviors effectively can make medical appointments more productive and reduce administrative burdens, allowing healthcare providers to focus more on patient-centered care.
Additionally, learning about difficult patients provides a clearer perception of the healthcare experience. It enhances understanding, reduces misunderstandings, and supports a holistic approach to care, considering not just physical symptoms but also emotional and psychological factors. This comprehensive view leads to better communication, more accurate diagnoses and treatments, improved problem-solving, and overall improved healthcare experiences for both patients and caregivers.
Now, an Introduction to Difficult Patients
Difficult Patients News – Imagine Jane, who arrives at her doctor’s office 15 minutes early, a fact she wears like a badge of honor. In her mind, punctuality is the hallmark of a good patient, a standard she prides herself on meeting. However, the landscape of healthcare has evolved significantly; being early is no longer the sole criterion for patient responsibility.
Today, the definition of a good patient extends far beyond mere punctuality. It encompasses being informed, prepared, and an active participant in one’s own care. Jane, with her refusal to fill out updated health forms and her disengagement during the consultation, starkly contrasts with this modern expectation. She represents a paradigm that is gradually becoming outdated in a healthcare system that now emphasizes patient education, proactive participation, and collaboration as key components of effective healthcare.
During her consultation, Jane remains disengaged, her arms crossed as she sits in the examination room. She meets her doctor’s questions with either terse nods or shrugs, her gaze drifting to the clock on the wall more often than not. When asked about her medical history or symptoms, her answers are vague, her tone suggesting she views these questions as unnecessary intrusions rather than tools for her wellbeing.
But what truly encapsulates the essence of the challenge is her preparedness – or lack thereof. Jane didn’t bring anything to take notes on, missing out on critical information regarding her treatment and care. This not only hampers her own health management but also creates additional strain on the healthcare system.
These so-called “Difficult Patients” like Jane represent more than just challenging interactions; they embody a fundamental disconnect in the healthcare journey. They are the catalysts that compel us to ask: What if there was a way to transform these difficult patients into cooperative and informed partners in their healthcare journey?
Enter Patient Better, a comprehensive health advocacy program designed to bridge these gaps. Through education and empowerment, Patient Better aims to reshape the patient-healthcare provider dynamic, facilitating a more efficient and effective medical landscape.
In the following sections, we will delve deeper into the characteristics of difficult patients, explore the root causes behind such behaviors, and illustrate, through a detailed side-by-side comparison, how these interactions typically unfold and the transformative potential of programs like Patient Better.
What are the Signs of a Difficult Patient?
Have you ever wondered if your approach to healthcare might be seen as challenging? While nobody intentionally becomes a difficult patient, certain behaviors can signal potential difficulties ahead in your care journey.
- Refusal to Complete Necessary Paperwork: Just like Jane in our earlier example, some difficult patients avoid filling out the requisite health forms. This can create medical and legal complications and increase administrative work for healthcare providers.
- Reluctance to Answer Routine Questions: A patient’s medical history and symptoms are crucial for correct diagnosis and treatment. Difficult patients often dodge these questions or provide vague answers, thereby compromising the quality of care they receive.
- Over-reliance on Electronic Health Records: While EHRs are useful tools, they don’t capture the full picture of a patient’s health. Difficult patients may rely too heavily on these records, dismissing the need for further discussion with healthcare providers.
- Not Bringing a Notebook or Means to Take Notes: As with Jane, difficult patients often come unprepared to document important aspects of their healthcare, such as medication regimens or post-op instructions.
These behaviors aren’t just frustrating; they’re counterproductive. They create unnecessary burdens on the healthcare system and can even lead to adverse patient outcomes. If these signs seem familiar, you’re likely dealing with difficult patients who require a different approach to healthcare management.
The Recognized Root Causes Behind Difficult Patients
Understanding the behaviors of difficult patients is just the tip of the iceberg; it’s equally essential to delve into the root causes behind such behavior. This insight is crucial for healthcare professionals who aim to transform these difficult experiences into more collaborative healthcare journeys. Here are some common reasons:
- Lack of Knowledge or Education on Their Condition: Often, difficult patients like Jane are not intentionally challenging; they simply don’t know any better. Lack of understanding about the significance of their health conditions can make them appear indifferent or uncooperative.
- Fear or Anxiety: Some difficult patients may be dealing with underlying anxieties related to their health or medical treatments, causing them to avoid discussions or refuse to comply with procedures.
- Mistrust of the Healthcare System: Given the complexities and intricacies of modern healthcare, it’s not uncommon for patients to become wary or distrustful. This skepticism can manifest as disruptive behavior, making it difficult for healthcare providers to offer appropriate care.
Recognizing these root causes is the first step toward transforming difficult patients into informed partners in their healthcare. These challenges call for a comprehensive solution that goes beyond the traditional physician-patient dynamic, introducing education and advocacy into the mix.
How Patient Better Addresses the Challenges of Difficult Patients
When dealing with difficult patients, healthcare professionals often feel like they’re walking a tightrope between providing quality care and managing time and resources efficiently. This is where Patient Better comes into play. Our comprehensive health advocacy program offers solutions that specifically target the root causes behind difficult patient behavior. Here’s how:
- Educating Patients to Be Proactive: Patient Better provides an educational program that empowers patients with the knowledge they need about their health conditions. Just imagine if Jane had been educated on why paperwork is essential, or why doctors ask certain questions; her approach to her healthcare journey would likely have been far more collaborative.
- Promotes Effective Communication: The program teaches patients and caregivers how to communicate effectively with healthcare providers, reducing misunderstandings and fostering mutual respect. Effective communication can turn difficult patients into engaged participants in their healthcare.
- Reduces Unfair Administrative Responsibilities: By making patients more informed and proactive, Patient Better alleviates common administrative problems such as incomplete paperwork, unpreparedness for appointments, and hesitance to answer medical questions. Thus, making the appointment more productive, reduces professional administrative burdens, and allows more focus on more important things, like patient-centered care.
Patient Better isn’t just about helping patients; it’s about creating an environment where healthcare professionals and patients can collaborate more efficiently and effectively. The program equips difficult patients with the tools they need to be better healthcare consumers, relieving stress and administrative burdens on healthcare professionals in the process.
Addressing the 10 Types of Difficult Patients Behaviors: Am I a Difficult Patient?
No one sets out to be labeled as a "difficult patient" in the healthcare system. Yet, stress, fear, misunderstanding, and poor communication can lead to behaviors that make medical interactions challenging for both patients and healthcare providers. Recognizing if you exhibit any of these behaviors is the first step towards transforming your healthcare experience from frustrating to collaborative.
This article explores ten common types of difficult patients, from the Demanding to the Silent, and provides practical strategies not only to avoid falling into these categories but also to enhance your interactions with your healthcare team. By understanding and adjusting your approach, you can become an empowered partner in your care, ensuring better treatment experiences and more favorable health outcomes.
The Demanding Patient: This patient type wants immediate attention and results, often having unrealistic expectations about the healthcare system’s capabilities and timing.
The Dependent Clinger: Overly reliant on medical staff for their emotional and physical needs, these patients often require a lot of time and reassurance, which can strain resources.
The Self-Destructive Patient: Engages in harmful behaviors towards themselves but refuses to accept care or follow medical advice, often denying the severity of their situation.
The Manipulative Patient: Tries to control the situation through guilt, anger, or bargaining; they may play off different team members against each other.
The Non-Compliant Patient: Frequently ignores medical advice, skips appointments, or doesn’t take their medications as prescribed, complicating their treatment plan and outcomes.
The Know-It-All: Believes they understand their health and treatment options better than the professionals, often challenging or openly disputing medical advice.
The Litigious Patient: Quickly mentions lawsuits and legal action, using intimidation to influence care, which can create a hostile environment for healthcare providers.
The Aggressive Patient: Exhibits hostile, violent, confrontational behavior, which can be verbal or physical; poses safety concerns for staff and other patients.
The Internet Researcher: Comes to appointments armed with loads of information (not always accurate) gathered from the internet and insists on discussing every piece of it.
The Silent Patient: Offers minimal information about their symptoms or history, which hampers the diagnostic process. Their reluctance can stem from fear, mistrust, or misunderstanding of the healthcare process.
Now, Let’s Perform a Side-by-Side Comparison of Difficult Patient Scenarios Examples
In our exploration of the challenges posed by so-called "Difficult Patients" in healthcare settings, it’s crucial to understand not just the theoretical aspects but also the real-world implications of such interactions. To bring this issue to life and offer a more tangible perspective, we present a side-by-side comparison exercise.
This exercise is designed to demonstrate the significant impact that a patient’s attitude and cooperation can have on the efficiency and effectiveness of a medical appointment. By contrasting an ideal scenario with the real-life example of "Jane," a difficult patient, we aim to highlight the various challenges healthcare professionals face and how these can ripple through the healthcare system, affecting not only the individual patient but also the overall functioning of healthcare facilities.
Our goal is to underscore the importance of patient education and proactive participation in healthcare, as well as to illuminate the potential benefits of programs like Patient Better. This comparison serves as a practical illustration of why transforming difficult patients into informed and cooperative partners is not just desirable but essential for the betterment of individual and collective healthcare experiences.
Let’s dive into the comparison to see how a typical medical appointment can unfold in different ways, depending on the patient’s approach and behavior.
A Real-World Scenario: Jane’s 2:00 PM Neurologist Appointment
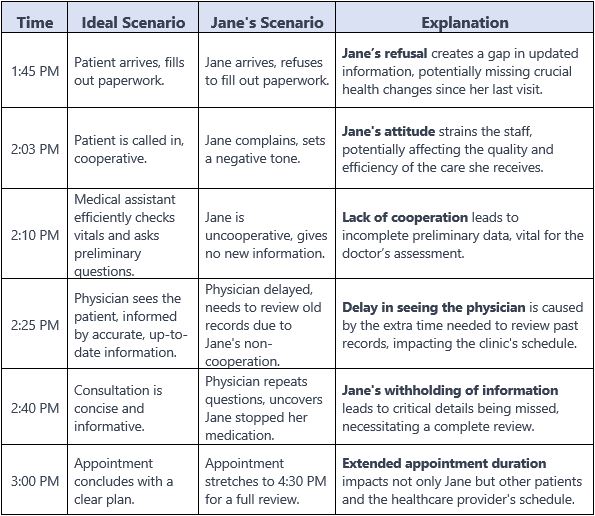
Key Takeaways:
Communication and Cooperation is Key: Jane’s lack of these elements leads to inefficiencies and frustrations, affecting the quality of care.
Continuously Updating Information Is a Must: Refusing to provide current information can have serious consequences for patient health and clinic operations.
Trusting the Healthcare System Essential: Such behavior not only impacts the individual patient’s care but also the functioning of the healthcare facility, affecting other patients and staff.
An Opportunity to Share Health Status is Empowering: This scenario illustrates the need for programs like Patient Better, which can educate and encourage patients to be proactive and cooperative, leading to better healthcare outcomes.
The Best Ways to Handle Difficult Medical Appointments
Dealing with challenging situations during medical appointments can be a real test, whether you’re a patient or a caregiver. Here are some practical tips to help you navigate these situations with confidence:
- Open Communication: When faced with a tough situation, start by establishing open and honest communication. Express your concerns and listen actively to the healthcare professional’s perspective.
- Be Informed: Take the initiative to educate yourself about your health condition or that of your loved one. Knowledge empowers you to ask relevant questions and make informed decisions.
- Prepare Questions: Before the appointment, jot down any questions or concerns you have. This helps ensure you cover all important topics during your visit.
- Advocate for Your Needs: Don’t be afraid to advocate for your healthcare needs or those of your loved one. Your input is valuable in creating a personalized care plan.
- Stay Calm: In challenging moments, try to remain calm and composed. Avoid confrontations, and focus on finding solutions together.
- Seek Support: Reach out to patient advocacy groups or support networks if you’re facing a particularly complex medical situation. They can provide guidance and resources.
- Follow-Up: After the appointment, stay engaged in your healthcare journey. Follow any instructions or recommendations provided by the healthcare professional.
- Tailored Care: Work with your healthcare team to create a care plan that suits your specific needs. Tailored care can lead to a more positive healthcare experience.
Remember, there’s no one-size-fits-all solution, and Patient Better is just one of many resources available. These strategies are designed to help you handle difficult medical appointments effectively. Feel free to adapt them to your unique situation, and don’t hesitate to seek additional support when needed.
Conclusion: Transforming Difficult Patient Encounters Into Positive Healthcare Partnerships
Facing the challenges of healthcare often feels like navigating a labyrinth—complex and fraught with unexpected turns. It’s in these moments that the signs of a difficult patient can inadvertently emerge. But what causes patients to be difficult? Is it fear, a lack of understanding, or perhaps previous difficult patient encounters that have left them wary?
At Patient Better, we recognize these signs and work diligently to address the root causes, transforming the difficult doctor-patient relationship into a harmonious alliance. Our approach is a beacon for both healthcare professionals and patients, illuminating the path to improved relationships and positive outcomes. We believe in the power of education to turn challenging patient scenarios into success stories of engagement and understanding.
How to be a better patient is no longer a question but a journey we facilitate. The ‘difficult patient’ becomes an archetype of the past as our participants learn to deal with difficult situations in healthcare with grace and knowledge. The transformation is profound: the demanding patient becomes an active listener, the know-it-all shares in the learning, and the non-compliant patient becomes a model of adherence.
As we unfold this narrative of change, Patient Better stands committed to guiding each individual toward becoming an informed partner in their healthcare. Embrace our program, and you will not only learn how to improve your relationships with healthcare professionals but also discover that being an empowered patient is the most rewarding role to play in the healthcare system.
Together, let’s redefine what it means to be a ‘difficult patient’ and celebrate every step toward becoming a proactive, knowledgeable, and collaborative partner in health. This is not just an opportunity—it’s your right. Patient Better is here to ensure that right is realized, one empowered patient at a time.
End of article.
Did you find this article useful and want to take the next step in becoming your own health advocate?
Stay in touch with us by connecting, liking, subscribing, reposting, or sharing with us on social media.
Disclaimer
The information provided here is for educational and entertainment purposes only. It is not intended as, nor should it be considered a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call 911 or your local emergency number.
Recommended Reads
If you found this article insightful, enhance your health advocacy journey with these carefully selected reads, chosen to deepen your understanding and empower your healthcare decisions.
Is learning a health advocacy program right for you?
Patient Better is a groundbreaking, all-in-one solution that empowers individuals to become recognized health advocates. With our comprehensive Health Advocacy Program, we provide aspiring advocates with the knowledge, skills, and resources needed to navigate the complexities of the healthcare system effectively. This unique program covers a wide range of topics, from understanding medical concepts, processes, and financial intricacies, to learning effective communication skills, patient advocacy techniques, and the importance of holistic wellness. Participants will emerge with a comprehensive skill set that enables them to navigate the healthcare landscape with confidence and positively impact their lives.
By enrolling in the Patient Better Health Advocacy Program, participants gain access to expert-led training sessions, interactive workshops, and real-world case studies. The curriculum is thoughtfully designed to equip advocates with practical tools to support patients and their families during challenging medical situations. As advocates, they learn to bridge the communication gap between healthcare providers and patients, ensuring that medical decisions are well-informed and aligned with the patient’s best interests.
Consider purchasing the Patient Better Health Advocacy Program if:
You or your family are facing challenges in communicating, coordinating, or collaborating on your healthcare efficiently and effectively.
You or your family have received a medical diagnosis and seek to minimize errors, oversights, and uninformed decisions.
You or your family are looking for a cost-effective solution to navigate and understand your health journey.
With the Patient Better Health Advocacy Program, you’ll gain the support and expertise needed to navigate the complexities of the healthcare system, empowering you to make informed decisions and improve your overall healthcare experience.
Coupon Code: Use HealthAdvocate10 for 10% off your purchase of the Patient Better Start-up Program and start your journey towards a more empowered and easier health journey.
For Search Engines
This article explores how individuals can transform from being perceived as difficult patients to empowered healthcare partners, enhancing their treatment experiences and outcomes. It provides practical strategies for improving communication with healthcare providers and actively participating in health care decisions. The purpose is to educate and empower patients to become proactive participants in their healthcare journey, ultimately fostering more effective and collaborative interactions with healthcare professionals. The article also highlights the role of Patient Better’s Health Advocacy Program in facilitating this transformation.

